Synthetic opioids continue to drive overdose deaths1
 Actor portrayals.
Actor portrayals. Actor portrayals.
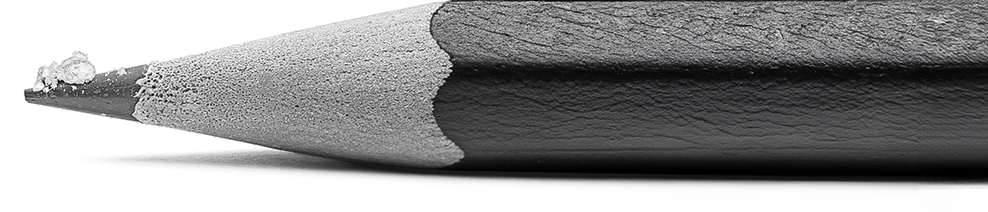
Actor portrayals.2 mg of fentanyl, a potentially lethal dose, can fit on the tip of a pencil.6
Artist rendering.
ZURNAI is indicated for the emergency treatment of known or suspected opioid overdose induced by natural or synthetic opioids in adults and pediatric patients aged 12 years and older, as manifested by respiratory and/or central nervous system depression.
ZURNAI is intended for immediate administration as emergency therapy in settings where opioids may be present.
ZURNAI is not a substitute for emergency medical care.
CONTRAINDICATIONS
ZURNAI is contraindicated in patients known to be hypersensitive to nalmefene hydrochloride or to any other ingredients in the product.
WARNINGS AND PRECAUTIONS
Risk of Recurrent Respiratory and Central Nervous System Depression
A recurrence of respiratory depression is possible, therefore, keep the patient under continued surveillance and administer repeat doses of ZURNAI if necessary, using a new auto-injector with each dose while awaiting emergency medical assistance.
Risk of Limited Efficacy with Partial Agonists or Mixed Agonist/Antagonists
Reversal of respiratory depression by partial agonists or mixed agonists/antagonists such as buprenorphine and pentazocine, may be incomplete. Repeat doses of ZURNAI may be required.
Precipitation of Severe Opioid Withdrawal
The use of ZURNAI in patients who are opioid dependent may precipitate opioid withdrawal.
Abrupt postoperative reversal of opioid depression may result in adverse cardiovascular (CV) effects. These events have primarily occurred in patients who had preexisting CV disorders or received other drugs that may have similar adverse CV effects. Monitor these patients closely in an appropriate healthcare setting after use of ZURNAI.
In neonates, opioid withdrawal may be
Risk of Opioid Overdose from Attempts to Overcome the Blockade
Attempts to overcome opioid withdrawal symptoms caused by opioid antagonists with high or repeated doses of exogenous opioids may lead to opioid intoxication and death.
ADVERSE REACTIONS
Most common adverse reactions (> 5%) are feeling hot, nausea, headache, dizziness, chills, vomiting, allodynia, palpitations, tinnitus, ear discomfort, feeling abnormal, burning sensation, hot flush, and irritability.
USE IN SPECIFIC POPULATIONS
Pregnancy
An opioid overdose is a medical emergency and can be fatal for the pregnant woman and fetus if left untreated. Treatment with ZURNAI for opioid overdose should not be withheld because of potential concerns regarding the effects of ZURNAI in the fetus.
Pediatric Use
The safety and effectiveness of ZURNAI for the emergency treatment of known or suspected opioid overdose, as manifested by respiratory and/or central nervous system depression, have not been established in pediatric patients younger than 12 years of age.
Geriatric Use
Clinical studies of nalmefene hydrochloride injection did not include sufficient number of subjects aged 65 and over to determine whether they respond differently from younger subjects.
Please read
To report SUSPECTED ADVERSE REACTIONS, contact Purdue Pharma L.P. at 1 888-726-7535, option 2, or FDA at 1-800-FDA-1088 or .
Intended for healthcare professionals of the United States of America only.
References: 1. Centers for Disease Control and Prevention. Provisional drug overdose data. CDC. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Published August 14, 2024. Accessed May 30, 2025. 2. Stokes EK, Pickens CM, Wilt G, Liu S, David F. County-level social vulnerability and nonfatal drug overdose emergency department visits and hospitalizations, January 2018-December 2020. Drug Alcohol Depend. 2023;247:109889. doi:10.1016/j.drugalcdep.2023.109889. 3. Friedman J, Hadland SE. The overdose crisis among US adolescents. N Engl J Med. 2024;390(2):97-100. doi:10.1056/NEJMp2312084. 4. Palamar JJ, Ciccarone D, Rutherford C, Keyes KM, Carr TH, Cottler LB. Trends in seizures of powders and pills containing illicit fentanyl in the United States, 2018 through 2021. Drug Alcohol Depend. 2022;234:109398. doi:10.1016/j.drugalcdep.2022.109398. 5. DEA. Fake pills fact sheet. www.dea.gov. https://www.dea.gov/sites/default/files/2024-11/DEA-OPCK_FactSheet_November_2024.pdf. Published November 2024. Accessed May 30, 2025. 6. DEA. One pill can kill. www.dea.gov. https://www.dea.gov/onepill. Updated May 19, 2025. Accessed May 30, 2025.